Honor, courage and commitment are the core values of the United States Marine Corps. However, federal prosecutors say that integrity vanished for hundreds of service members involved in one of the military’s biggest fraud conspiracies in recent memory. The U.S. government has never revealed what discipline, if any, they received and won’t answer any questions about where they are now.
Federal charging documents go into great detail about the elaborate and lucrative scheme, in which a compounding pharmacy out of Utah filled phony prescriptions written by a Tennessee clinic as part of a fake medical study.
If the commands took no action in a case like this, then they’re sending the wrong message to other Marines in the unit.
Gary Barthel, defense attorney
Those prescriptions went for big money. When the conspiracy reached full swing, the clinic billed TRICARE, the government-sponsored military health care system, more than $10,000 per prescription, sometimes upward of $20,000. This wasn’t life-saving medication – rather, often the pharmacy filled prescriptions for cosmetic creams, like stretch marks and sunscreen, or a “general wellness tablet.”
Get top local stories in San Diego delivered to you every morning. >Sign up for NBC San Diego's News Headlines newsletter.
To find sham patients, four Marines and one sailor acted as recruiters to identify service members and their families who knowingly participated in the scheme in exchange for $300 monthly kickbacks. More than 350 Marines and military family members played ball. The vast majority were based at the Marine Corps Air Station in Miramar.

“It took very little work to sign people up to receive free money,” Joshua Morgan, one of the (now former active-duty) Marine recruiters, told prosecutors.
Local
Retired Marine and defense attorney Gary Barthel often represents service members caught up in similar schemes. With 40 years of experience in military law, the former military court martial prosecutor has also served as a legal advisor to commanding generals.
“The temptation is there,” Barthel said. “They’re young. They’re hurting for money, and they’ll jump on the opportunity.”
Barthel told NBC 7 he was initially shocked at the allegations against hundreds of San Diego active-duty Marines but said it's not unusual for service members to be recruited into criminal enterprises.
“Especially young enlisted service members,” Barthel said, “they don’t get paid a lot of money. It’s easy for them to look the other way. Marines are typically trained to take risks, and so it becomes easy for them to do that.”
The conspiracy was a successful one, launching in 2014 and hauling in $65 million. The key players, the married clinic owners, spent that money on a lavish lifestyle. Prosecutors say that included an 82-foot yacht, two Aston Martins, gold and silver bars, dozens of pieces of farm equipment, tractor-trailer trucks and three pieces of real estate in Tennessee.
'Opened up the floodgates for fraud'
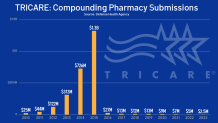
The clinic owners weren’t the only ones who figured out how easy it was to steal from Uncle Sam. Dozens of other clinics and pharmacies were treating TRICARE like a personal piggy bank. The spike in bogus prescriptions for compounded drugs left the military health care program with a $2 billion problem seemingly overnight. It was so bad, TRICARE nearly declared bankruptcy.
So how did we get here?
In 2012, TRICARE changed its policy for compound prescriptions, which are custom-made medications specifically created for patients. They are commonly prescribed when a medicine, ingredient or dose isn’t commercially available. For example, if a patient is allergic to an ingredient in a common prescription.
In 2012, TRICARE allowed pharmacies to charge for each individual ingredient. The Department of Defense said that “opened up the floodgates for fraud.” Before 2012, the average compounding pharmacy prescription was $100. Within two years, the average cost of a 30-day supply skyrocketed to $13,000.
The fraud scheme ends
The fraud came to a halt about a year later after a nationwide crackdown on organized fraud schemes surrounding bogus compound prescriptions resulted in dozens of indictments across the country.
That brings us back to San Diego. The Department of Justice indicted 11 people. All pleaded guilty and were sentenced.
The mastermind of the scheme, clinic owner Jimmy Collins, got a 10-year prison sentence. He and his co-conspirator wife, Ashley, were also ordered to pay back the $65 million. The two doctors writing the fake prescriptions were sent away for two years, and the five recruiters got between 6- and 21-month sentences.
The Department of Justice sent out more than a dozen press releases about the case, touting its investigation and its results, but there were glaring absences from those releases: Any details about the discipline directed at hundreds of Marine sham patients.
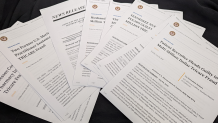
There were no details about prosecutions, plea deals, sentences, dishonorable discharges, demotions, letters of reprimand, monetary restitution or fines.
Federal indictment documents leave little doubt that the sham patients were indeed aware of the fraud scheme. They state that the Marine recruiters “directed the straw TRICARE beneficiaries to falsely represent on a pre-printed form that they had seen a doctor … the beneficiaries had neither seen nor spoken to any medical professional regarding the compounded prescription medications prescribed to them.”
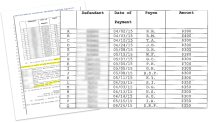
And prosecutors seemingly knew exactly who these Marines were. Documents show the recruiters kept detailed logs of their kickback payouts to the sham beneficiaries, making the work much easier for prosecutors to put the pieces together.
Starting in January, NBC 7 Investigates repeatedly asked the Office of the U.S. Attorney of the Southern District of California and the U.S. Department of Justice whether the government plans to file any criminal charges against the Marines who accepted fake prescriptions for kickbacks.
A spokeswoman said the Department of Justice would not discuss the case beyond what they drafted in their news releases and sent us this statement:
“The United States prosecuted multiple individuals, including some service members, who had key roles in the scheme to defraud, knew about and understood the scheme and intended to defraud Tricare. The Department of Justice has a long-standing practice of not confirming, denying or commenting about investigations or inquiries regarding individuals not charged with a federal crime.”
A representative for MCAS Miramar told NBC 7 to contact the Department of Defense, which in turn told us to file a Freedom of Information Act request with the U.S. Marine Corps, which we did. However, these types of public record requests often take more than a year to process.
The Naval Criminal Investigative Service also declined to provide any information about service member discipline.
Military law expert Barthel told us not to hold our breath on answers.
“The Department of Justice is not going to prosecute those service members,” Barthel said. “They’re going to go for the kingpins involved in the conspiracy.”
Even though the $65 million scheme wouldn’t have been possible without the help of those rank-and-file Marines.
“They would not have been able to commit those crimes if they didn’t have the 350 other people down there being paid kickbacks to get these prescriptions written,” Barthel said. “I would be shocked if the commands took no action, no disciplinary action.”
It’s possible the Marines faced consequences in military court, though NBC 7 couldn’t find that information in publicly available courts martial filings.
“It really does put a black eye on the organization, on the military institution,” Barthel told NBC 7. “If the commands took no action in a case like this, then they’re sending the wrong message to other Marines in the unit. That, in other words, you can get away with this.…They’re not only robbing service members and veterans from their health insurance, but they’re also robbing taxpayers from dollars.”
Changes to TRICARE
The Defense Health Agency manages TRICARE. NBC 7 also asked them for an interview for this story, which they declined. However, a spokesman sent us a statement that detailed changes in how compounding pharmacies are reimbursed for prescriptions.
In May 2015, DHA instituted a screening process for all ingredients in compound prescriptions. Ingredients not known to be safe, effective and medically necessary are not cost-shared. This screening process is similar to what Pharmacy Benefits Manager, Express Scripts, instituted for their commercial clients. These measures resulted in a 98% reduction in cost.
In addition to instituting robust screening measures when appropriate, DHA invoked temporary claims payment suspensions.
In general, temporary claims payment suspensions may be invoked to protect the interests of the government for a period reasonably necessary to complete investigation or necessary appropriate criminal, civil and administrative proceedings.
Prior authorization requirements were also put into place as a safeguard for legitimate compounds to review ingredients and allowing the beneficiary’s physician to present evidence that the compound is safe, effective and medically necessary.
Additionally, following the spike in April 2015, DHA began administrative audits of compound pharmacies to verify the validity of compound pharmaceutical claims. Audits include provider and pharmacy inquiries in addition to detail claims reviews, and any overpayment identified during this process were recouped.
Finally, the Department of Justice, in collaboration with DHA and the Defense Criminal Investigative Service, established the Compound Pharmaceutical Fraud Task Force to take on civil and criminal investigations into pharmacies, physicians and marketers involved in the compound pharmacy scheme.
By statute, DHA/TRICARE may recover single dollar losses from civil settlements. Double or treble damages, fines or penalties allowed in civil settlements are returned to the U.S. Treasury. Settlement recoveries are applied to TRICARE benefit dollars for the year the money is received.
Since 2013, TRICARE, with the assistance of ESI, our pharmacy benefit contractor, has recouped $35,812,489 from compounding pharmacies.



